Èñòî÷íèê: http://www.springerlink.com/content/1750402227356l86/fulltext.pdf
Obstetrical and Pediatric Anesthesia Baseline heart rate may predict hypotension after spinal anesthesia in prehydrated obstetrical patients
Purpose: Hypotension is the most frequent complication of spinal anesthesia in pregnant patients. This study was designed to identify patients at risk for postspinal hypotension based on preoperative vital signs before and after an orthostatic challenge.
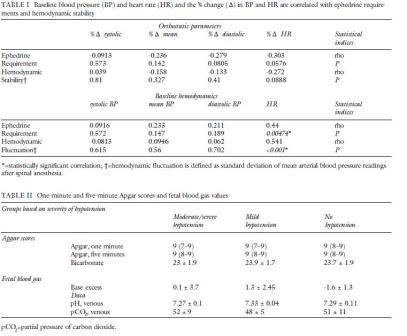
Methods: Forty healthy women scheduled for elective Cesarean section were enrolled in this prospective trial. Blood pressure (BP) and heart rate (HR) were recorded with the patient in the lateral supine position and after standing up. After a bupivacaine spinal anesthetic, BP was obtained every two minutes for 30 min. Ephedrine treatment was administered based on the degree of hypotension observed. Hemodynamic parameters were correlated to ephedrine requirements (Spearman's rank order correlation).
Results: There was a significant correlation in baseline maternal HR and ephedrine requirements (P=0.005). The degree of orthostatic changes in mean arterial BP and HR did not correlate with postspinal hypotension.
Conclusions: Baseline HR may be predictive of obstetric spinal hypotension. Higher baseline HR, possibly reflecting a higher sympathetic tone, may be a useful parameter to predict postspinal hypotension.
MATERNAL hypotension is a well-recognized side effect of spinal anesthesia. In the obstetric population, this may compromise the welfare of both mother and fetus.1 Hypotension can be prevented to some extent with prophylactic ephedrine, 2 pelvic tilt, and intravascular volume expansion. The use of combined prophylactic measures can decrease the incidence of hypotension3 but there are potential risks associated with this therapy: reactive hypertension4 and cardiac arrhythmia have been reported with the use of ephedrine, and pulmonary edema may result from excessive hydration. This study was designed to evaluate whether blood pressure (BP) and heart rate (HR) obtained prior to spinal anesthesia (SA) in the supine and standing position would be useful to predict a subset of pregnant patients that might be at high risk for postspinal hypotension.
Methods
This study was approved by our Institutional Review Board. Forty healthy patients scheduled for elective Cesarean section were enrolled on the day of surgery after written informed consent was obtained. Patients with a history of medical conditions that might affect the cardiovascular system and patients with a body mass index >30 kg·m2 were excluded.
Baseline BP and HR were obtained in the preoperative holding area by calculating the average of five independent readings taken in the lateral supine position. Patients received 30 mL sodium citrate by mouth and were hydrated with 15 mL·kg-1 Ringer's lactate. Immediately prior to the SA, subjects were asked to stand up from a recumbent position on the stretcher. Without delay, five noninvasive BP and HR recordings were obtained every minute in sequence and averaged.
With standard monitors in place SA was performed in the sitting position using a 25-GA Whitacre needle and 12 mg hyperbaric bupivacaine with 10-?g fentanyl and 0.3 mg preservative free morphine. Patients were then placed supine with a 15% pelvic tilt. Noninvasive BP recordings were obtained every two minutes for 30 min and every five minutes thereafter.
The treatment of hypotension was based on the decrease in mean arterial blood pressure (MAP) relative to baseline. A MAP decrease of >20% but <30% was treated with 5 mg iv ephedrine. A MAP decrease >30% was treated with 10 mg ephedrine iv. Ephedrine treatment was repeated every two minutes as indicated. The amount of ephedrine administered within 30 min after SA was used to calculate ephedrine requirements. Hemodynamic fluctuation was defined as standard deviation of post-SA MAP recordings and was used as an indicator of hemodynamic instability. Conversely, patients with little fluctuation in BP after SA were considered hemodynamically stable.
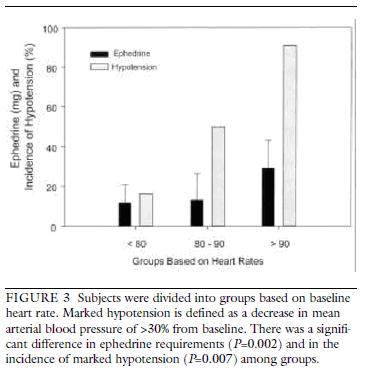
We performed two post-hoc analyses. In the first, we divided subjects into groups based on the observed degree of postspinal hypotension to examine the possible effect of hypotension on fetal blood gas or Apgar scores. In this analysis, mild hypotension was defined as a decrease in MAP of >20% but <30% of baseline and marked hypotension was defined as a decrease in MAP >30% of baseline. In the second analysis, we divided subjects into three groups based on the subject's baseline HR (<80 beats·min- 1, 80 to 90 beats·min- 1 and >90 beats·min-1). We then calculated ephedrine requirements and the incidence of marked hypotension for those groups.
The sample size calculation for this study was based on our objective to define a correlation in baseline hemodynamic data and the observed degree of hypotension. Assuming a correlation coefficient of 0.45 we needed 40 patients to obtain 80% power at a significance level of 0.05 (alpha). The Spearman's rank order correlation was used to calculate correlations of hemodynamic parameters and hypotension (ephedrine requirement) because several data subsets failed the normality test. Baseline and standing hemodynamic data were compared using Student's t test. We used a one-way ANOVA and the Tukey post-hoc test to analyze ephedrine requirements among groups based on baseline HR. The incidence of hypotension among groups was compared using a chi-square test. We used a one-way ANOVA to compare fetal blood gas data and the Kruskal-Wallis test to compare Apgar scores. A Pvalue of 0.05 was considered statistically significant.
Results
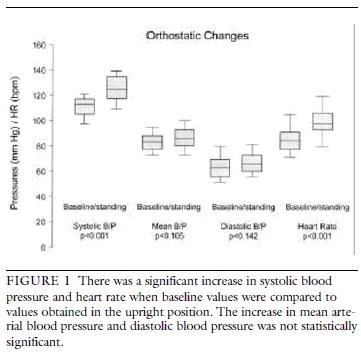
Systolic BP and HR increased significantly with the orthostatic challenge (Figure 1). Over the 30 min observation period following SA no hypotension was observed in six subjects (15%), mild hypotension in ten (25%), and moderate to marked hypotension in 24 subjects (60%). There was a significant positive correlation in baseline HR and ephedrine requirements (P=0.005, Table I and Figure 2). HR also correlated with hemodynamic fluctuation (standard deviation of post-SA
MAP, P<0.001, Table I and Figure 2). With increasing HR, the ephedrine requirement and the incidence of hypotension increased. This is illustrated in Figure 3; subjects with a baseline HR rate greater than 90 beats·min-1 had an 83% chance (positive predictive value) of developing marked hypotension after SA and patients with a HR less than 90 beats·min-1 had a 75%
chance (negative predictive value) of not developing marked hypotension. Choosing a HR of 80 beats·min-1 as cut-off, the positive predictive value was 18% (chance of developing hypotension) with a 52% negative predictive value. There was no significant correlation in the
observed orthostatic change for hemodynamics and hypotension (ephedrine requirements). There was no significant difference in fetal blood gases and Apgar scores when comparing patients in three groups based on the degree of hypotension observed (Table I).
Discussion
Pregnancy is associated with profound changes in maternal hemodynamics. The autonomic nervous system plays a central role in the adaptation of the cardiovascular
system to various hemodynamic requirements and is the principal system involved in
short-term cardiovascular control. The cardiovascular response to an orthostatic stress has been used for the assessment of intravascular volume status.7
Standing from the supine position causes the blood to pool from the thorax into the lower extremity veins. In nonpregnant subjects this may cause a fall in central venous filling pressure (preload), a decline in stroke volume, and cardiac output.8The decrease in BP caused by standing unloads systemic baroreceptors and, therefore, increases the HR. Decreased stimulation of high-pressure baroreceptors, as the arterial BP decreases, leads to reflex vasoconstriction
and an increase in BP.
Normally, the diastolic BP increases by about 10 mmHg while the systolic BP remains relatively stable. The HR increases by 10 to 20 beats·min-1 in nonpregnant women.9 The immediate decrease in the systolic BP caused by tilting diminishes during the lasts month of pregnancy.1 0 Increased sympathetic efferent activity to the blood vessels, induced by the upright position, may explain the BP increase after standing. The increase in BP may also be due to a smaller decrease in stroke volume in the upright position.1 1 The increased intravascular volume probably explains this change.
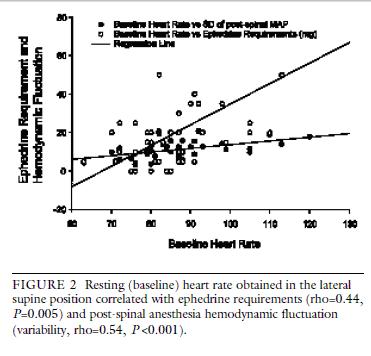
We postulated that the orthostatic cardiovascular reflexes in pregnancy might be used to identify patients at risk for hypotension after SA. In fact, the pathophysiologic mechanisms of hypotension after SA are similar to those causing orthostatic hypotension; decreased venous return and decreased arteriolar resistance. 1 2 This was also the basis for a study by Kinsella et al.1 3 who attempted to predict hypotension during elective Cesarean section using a modified orthostatic challenge, the tilt test. Like Kinsella and coworkers, we could not establish a correlation in the observed change in BP or HR and post-SA hypotension. Unlike Kinsella et al., we correlated baseline BP and HR with ephedrine requirements. We found a significant correlation in baseline HR and ephedrine requirements and in hemodynamic fluctuation after SA (Figure 2). A higher baseline HR in pregnant women scheduled for elective Cesarean section using SA was associated with more hypotension and less hemodynamic stability. We believe that a higher baseline HR reflects the subject's higher sympathetic tone. Individuals with high intrinsic sympathetic tone might be at greater risk for a more pronounced decrease in BP as a result of the spinal sympathectomy. Hence, the association of increased HR with post-SA hypotension. This finding may have some practical implications and questions whether pregnant patients with higher HR should be expected to be at higher risk for hypotension. This subset of patients might also benefit from better prophylactic measures to reduce the incidence of post-SA hypotension.
In contrast to the cardiovascular orthostatic response in non-pregnant women, we have observed a significant increase in systolic BP and only a minor increase in diastolic BP with the orthostatic challenge. During pregnancy, central venous pressure after standing remains practically unchanged1 4 and the HR reaction appears to be more pronounced, which suggests an increased sympathetic outflow to the heart.1 5 In summary, this study confirms the increase in HR and BP in response to an orthostatic challenge in the pre- hydrated pregnant patient. Baseline HR prior to hydration, rather than the orthostatic change in BP, may be useful to predict post-SA hypotension in the obstetric patient.