The PROforma
guideline specification
language:
progress and prospects
Bury, J., Fox, J., Sutton, D.
Advanced Computation Laboratory,
Imperial Cancer
Research Fund, London, UK.
{jb,jf,ds}@acl.icnet.uk
Abstract. Medical guidelines are constructed
with the aim of
assisting
clinicians in making decisions that are informed by the best available
medical
evidence. In order to achieve this aim, they must be disseminated in a
form
that makes them easy for clinicians to use and easy for domain experts
to
critique. Furthermore, the language
in which they are expressed must
facilitate their
transfer between institutions and their adaptation to local conditions.
This
paper describes PROforma, a
knowledge representation language
that
attempts to meet these desiderata. PROforma
is formal knowledge
representation language designed to capture the content and structure
of a
clinical guideline in a form that can be interpreted by a computer. The
language embodies many contemporary themes in machine interpretable
guideline
representation schemas whilst retaining some distinctive features. This
paper
describes the key features of the PROforma
language in the
context of
recent trends and developments in the field of electronic guideline
representation
formats. We describe our experiences in applying PROforma
to a
range of
clinical decision making and workflow problems, and the benefits and
limitations
of the current language specification are discussed. Finally, we
outline plans
for the further refinement of PROforma.
Keywords :
Decision support systems, Clinical
guidelines,
Knowledge engineering, PROforma.
1 Introduction
This paper describes the key features of
the PROforma
language in the context of
recent trends and developments in the
field of
electronic guideline representation formats. The structure of the paper
is as
follows: Section 2 outlines the problems that clinical guidelines
address and
section 3 explains the paradigms that have arisen for the expression of
such guidelines.
Section 4 describes the theoretical basis of PROforma.
2 Guidelines and workflow
The explosion of interest in developing
and publishing
clinical guidelines, both using conventional media and on the World
Wide Web,
is an indicator of the growing importance attached to clinical
guidelines in
medicine. Kohn et al.[1] describe the recent estimate from the US
Institute of
Medicine that there may be as many as 98,000 unnecessary deaths per
annum resulting
from avoidable clinical error, which suggests there is a genuine need
for such
guidelines. The vast majority of clinical practice guidelines are
published as
text, and typically include criteria describing their applicability to
particular groups of patients, the recommended processes of care,
appropriate
use of materials and procedures and so on, as well as providing
ancillary
information such as supporting evidence. Clinical guidelines are
generally
concerned with two main areas that directly affect the quality and
effectiveness of patient care: the quality of clinical decision-making,
and the
correct and timely management of clinical tasks. A clinical guideline
thus
incorporates information relating to both decision-making and workflow
management.
2.1 Decision-making: What to believe and
what to do
Decision theory describes two main
classes of
decision: those concerning what to believe
(e.g. what is wrong
with a
patient, how serious a disease is, the possible prognosis) and those
concerning
what to do (e.g.
whether or not a patient should be referred
for
specialist care, what treatment or treatment strategy is appropriate,
whether
tests or investigations are required). Both of these classes of
decision are
vulnerable to many kinds of error. Errors in diagnosis or prognosis
decisions
can result from the absence of critical information about a patient, or
difficulties in assessing relative strengths of evidence for example.
Errors in
treatment and other management actions can result from incorrect
decisions
about eligibility or failures to allow for possible drug interactions,
etc.
2.2 Task management: Who does what,
when, how and
where
Even assuming that all clinical
decisions are taken
correctly, there are still countless ways in which errors can be made,
and
which can be costly in terms of the efficacy or efficiency of patient
care.
Tasks may be inadvertently omitted, carried out too late or adverse
events may be
missed. More complex clinical procedures such as care pathways or
chemotherapy protocols
may be carried out over an extended timescale by multiple healthcare
providers,
resulting in further potential hazards e.g. through a failure to keep
sufficiently complete clinical records or ensure that staff in the care
team
are kept informed about actions that have been carried out or are
planned.
2.3 Delivering Clinical Guidelines
While the systematic preparation and
publication of
clinical guidelines is of great importance, it is only a first step
towards
ensuring consistent compliance with the standards of care represented
in those
guidelines [2]. A guideline may set out current best-practice in great
detail,
but if clinicians do not have time to access the guidelines, or fully
absorb
their content and apply it correctly in their decision-making, or the
clinical
organisation fails to ensure that all the required tasks are carried
out in a
timely manner, then the objectives of the guideline may not be
reflected in
clinical outcomes.
From an AI perspective there is an
obvious alternative
to publishing guidelines solely in human readable form such as text,
tables or
flow diagrams, which is to formalize the medical knowledge contained in
these
guidelines in a form that a computer can apply to support clinicians in
their
routine work. The PROforma guideline
specification language and
its
associated software attempt to provide such a formal framework. In this
paper
we describe the PROforma language
in the context of recent
trends in
guideline representation, review the experience we have gained in
applying PROforma
technology in a variety of
clinical domains, and present our plans
for the
future development of PROforma.
3 Paradigms for representing clinical
guidelines and
workflow
3.1 The procedural approach
Early computerised clinical support
systems, including
decision support systems such as statistical decision aids and clinical
algorithms, whether expressed as conventional programs or in visual
notations
such as flow diagrams, did not separate the clinical knowledge from the
computation details of how that knowledge was to be delivered.
Although such systems can be
satisfactory, many
limitations of the procedural approach have been identified in the AI
and
knowledge engineering literature. First of all users, particularly
non-programmers, find it difficult to comprehend the underlying
clinical logic
by simple inspection of a computer program. Second, maintaining the
guideline
software as medical knowledge increases is notoriously difficult, and
such systems
lack reusability -
the knowledge they embody cannot be readily
exported
to other systems in a modular form. As a consequence it is increasingly
recognised that a better way of representing medical knowledge is in declarative
form, which allows knowledge of
medical concepts such as diseases,
drugs and
tests to be clearly separated from the reasoning and problem-solving
processes
that use that knowledge in particular medical contexts.
3.2 Rule based systems
Rule based expert systems such as MYCIN
[3] and
Oncocin [4] reflected the recognition of the importance of declarative
knowledge representation and pioneered a significant change in the
development
of clinical decision support systems in the 1970s and ‘80s.
Such
systems
clearly separated domain-specific knowledge expressed as sets of rules
from the
generalised inference engine, typically a backward-chaining or
forward-chaining
system, which would apply those rules. This represented a paradigm
shift in the
construction of decision support systems, and promised improved
readability,
modularity and reusability of the knowledge bases. However, despite the
popularity and technical elegance of rule based systems, and the
enhanced
readability they have brought, they have been less successful in
achieving
modularity and reusability of knowledge. In practice rules can be
written in a procedural
way and frequently depend upon being carefully crafted to ensure that
they are only
applied in specific situations making their transfer to other
applications
difficult [5] and potentially hazardous, as demonstrated in studies
with the
Arden syntax [6], which can be viewed as a hybrid of simple rule-based
and more
traditional procedural methods.
3.3 Task based systems
The limitations of rule-based systems
have led to the
recent emergence of a further paradigm shift in the development of
clinical
knowledge systems. Here, rule-based and task-based formalisms are
combined to
represent clinical processes. How a particular logical condition should
be
interpreted and acted upon depends, for example, on whether that rule
represents
part of a diagnostic process, a precondition for a particular clinical
intervention,
or a contraindication to a particular drug therapy. Task-based systems
therefore
attempt to contextualise rules within explicit and intuitive models of
the
clinical process with the aim of combining the programmatic richness of
a
procedural representation with the logical clarity of declaratively
expressed
knowledge.
Use of an intuitive representation of
the clinical
process has at least two potential advantages. Firstly, building the
knowledge
base should be an easier process for domain experts to participate in,
given
that tasks provide a higher-level and more intuitive set of design
primitives
than conventional programming languages or languages based on rules.
Secondly,
systems built around this approach have the potential to integrate into
the
clinical environment and workflow more easily, based as they are around
primitives which correlate with real world concepts and processes
familiar to
users. PROforma [7]
is one example of a task-based guideline
representation format. Other schemas that embody some or all of the
features of
the paradigm include the Guideline Interchange Format (GLIF), developed
by the
Intermed Collaboratory [8], SMART [9], Eon [10], and the Asgaard
Project [11].
4 PROforma
– a task based
approach to
guideline
representation
The term “Clinical
Guidelines” describes a
heterogeneous range of textual material designed to support
practitioners in
their decision-making. Individual guidelines may describe interventions
concerning populations or individuals. These interventions may be
simple
“atomic” actions or complex plans of therapy to be
conducted over time. The decisions
they describe include diagnostic, prognostic, therapeutic and risk
assessment decisions.
Unlike clinical protocols, which are intended to be followed rigidly,
usually within
special contexts such as clinical trials, clinical guidelines often
outline
general principles of management, to be considered by experienced staff
as they
exercise their clinical judgement. Guidelines therefore frequently
contain
ancillary information such as the evidence and literature on which
their
recommendations are based, guideline authorship, and the statements of
the
applicability of the material presented to particular patient groups.
When work began on PROforma
in the early 1990s,
the main requirements for the language were that it should:
·
Be sufficiently expressive to fully
represent a range
of clinical processes
·
Be sufficiently general to describe
processes in any
clinical specialty, from routine care to clinical research
·
Use concepts that are intuitive for
clinical users whilst
ensuring that
·
Processes specified in the language can
be enacted by
machine
·
The semantics of the language are
demonstrably sound
·
Applications can be automatically
checked for
consistency and other properties PROforma
combines the features
of a
formal specification language as developed in software engineering with
the
features of knowledge representation languages as developed in
artificial
intelligence. The PROforma
language structure is based on
a simple
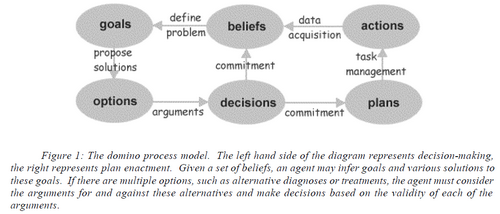
but versatile clinical process model referred to as the domino
model.
This model was abstracted from a variety of empirical studies of
clinical
decision-making and the development of aids to support patient
management. The
logical form of the domino model is shown in figure 1.
As described earlier, decision-making is a core function of any guideline representation and enactment schema. Statistical decision theory is the most formal decision model but in many respects has proved difficult to use and unattractive to clinicians. Decision theory based on mathematical probabilities is sound and well understood, but decision support systems based on statistical decision theory are often inflexible and difficult to use, and of limited applicability to knowledge-rich domains such as healthcare where precise parameters like quantitative probabilities are seldom known.
Discussion and conclusions
We believe that the task based paradigm represents a promising solution to the problem of developing guideline representation formats that maintain a declarative knowledge base whilst reflecting the constraints of the clinical workflow and process within which that knowledge is to be applied. We have found the particular task model adopted in PROforma to be both expressive and intuitive, with its simplicity and formal foundations being significant benefits. Although the development of the PROforma task model appears to have been productive, we must now address a second set of challenges. The technical challenges of providing interfaces between decision support systems and other clinical information systems such as electronic patient records and laboratory systems are well known. Within the context of the PROforma 2000 project, the definition of a clear API for PROforma technologies will be a first step towards supporting communication between PROforma and other systems. We also hope that the adoption of techniques from the agent-based paradigm will help to address the difficulties of communication and negotiation between guidelines, and facilitate the development of clearer behavioural semantics for goal-based guideline representation.
The development of more intelligent functions, such as plan repair and the dynamic modification of plans represents a longer term objective for the PROforma format. These features will require a deeper understanding of general cognitive functions and how thesecan be modelled in formal systems. A further challenge in providing decision support at the point of care is in integrating computer systems into the dynamic of the clinical consultation. We are exploring the notion of “use models”, in which we consider the impact of a computer on the complex discourse between patient and clinician. Introducing a computer as a “third party” in this discourse may have significant effects on the psychological aspects of the consultation, both for clinicians and patients. If the decision support systems we wish to provide are to be integrated into clinical practice, their design must support the subtleties of the human relationship that exists between patients and their clinicians so that they may enhance, rather than detract from, this relationship.
Acknowledgements
We thank Richard Thompson, Ali Rahmanzadeh, and Christian Blum for their help in preparation of this manuscript.
References[1]
Kohn, L., Corrigan, J., Donaldson, M. (Eds). To Err is Human: Building
a Safer Health System. National Academy Press, Washington, D. C., 1999.
[2] Shiffman RN, Brandt CA, Liaw Y, Corb GJ, 1999. A design model for
computer-based guideline implementation based on information management
services. J Am Med Inform Assoc 1999; 6(2):99-103
[3] Wraith SM, Aikins JS, Buchanan BG, Clancey WJ, Davis R, Fagan LM,
Hannigan JF, Scott AC, Shortliffe EH, van Melle WJ, Yu VL, Axline SG,
Cohen SN. Computerized consultation system for selection of
antimicrobial therapy. Am J Hosp Pharm 1976; 33(12):1304-8
[4] Shortliffe EH. Update on ONCOCIN: a chemotherapy advisor for
clinical oncology. Med. Inform. 1986; 11(1):19-21
[5] Shwe M, Sujansky W, Middleton B. Reuse of knowledge represented in
the Arden syntax. Proc Annu Symp Comput Appl Med Care 1992; 47-51
[6] Hripcsak G, Wigertz OB, Kahn MG, Clayton PD, Pryor TA. ASTM E31.15
on health knowledge representation: the Arden Syntax. Stud Health
Technol Inform 1993;6:105-12
[7] Fox J, Johns N, Rahmanzadeh A, Thompson R. PROforma: A method and
language for specifying clinical guidelines and protocols. In: J
Brender, J P Christensen, J-R Scherrer P McNair (eds) Medical
Informatics Europe '96 IOS Press, Ams terdam 1996 pp. 516-520.
[8] Ohno-Machado L, Gennari JH, Murphy SN, Jain NL, Tu SW, Oliver DE,
Pattison-Gordon E, Greenes RA, Shortliffe EH, Barnett GO. The guideline
interchange format: a model for representing guidelines. J Am Med
Inform Assoc 1998; 5(4):357-72
[9] Pisanelli DM, Consorti F, Merialdo P , SMART: a system supporting
medical activities in real-time. Stud Health Technol Inform 1997; 43 Pt
A:343-7
[10] Tu SW, Musen MA. A Flexible Approach to Guideline Modeling. AMIA
1999 Annual Symposium, Washington D.C., 420-424. 1999.
[11] Shahar Y, Miksch S, Johnson P. The Asgaard project: a
task-specific framework for the application and critiquing of
time-oriented clinical guidelines. Artif Intell Med 1998; 14(1-2):29-51