← Home
A Leahy, K Besherdas, C Clayman, I Mason, O Epstein
Gastric dysrhythmias occur in gastro-oesophageal
reflux disease complicated by food regurgitation
but not in uncomplicated reflux
Abstract
Aim—To investigate gastric pacemaker
activity in gastro-oesophageal reflux disease
using the electrogastrogram.
Patients—Forty patients with gastrooesophageal
reflux disease (20 with acid
reflux, 20 with the additional symptom of
food regurgitation) and 30 asymptomatic
controls.
Methods—Patients were studied using an
electrogastrogram, oesophageal manometry,
and 24 hour ambulatory oesophageal
pH analysis.
Results—An abnormal electrogastrogram
was recorded in two (7%) controls, two
(10%) patients with acid reflux, and 10
(50%) patients with food regurgitation.
Food regurgitators had significantly more
gastric dysrhythmias (tachygastrias) both
before (p<0.02) and after (p<0.01) a test
meal. Gastric pacemaker activity was also
significantly less stable following the test
meal in food regurgitators (p<0.003).
Patients with food regurgitation and an
abnormal electrogastrogram had higher
oesophageal acid exposure than those with
a normal electrogastrogram (p<0.05).
Conclusions—The electrogastrogram is
usually normal in gastro-oesophageal reflux
disease but an abnormal rhythm
occurred in half of our patients with the
additional symptom of food regurgitation.
Furthermore, an abnormal electrogastrogram
is associated with increased
oesophageal acid exposure.
The electrogastrogram (EGG) is a noninvasive
method of recording gastric myoelectrical
activity. The activity is detected by
positioning cutaneous electrodes over the
upper abdomen and capturing the mean
electrical frequency of the gastric pacemaker.
Normal gastric myoelectrical activity consists
of a slow wave and spike potentials. The EGG
records the slow wave, which controls the
velocity and propagation of gastric contractions.
This oscillates within a narrow frequency
band, and any gastric activity outside this band
is designated a dysrhythmia.
Gastric dysrhythmias consist of fast frequency
(tachygastrias) and slow frequency
(bradygastrias) waves. Studies using serosal
transducers and manometry have shown that tachygastrias correlate with absent antral contractions.
Bradygastrias have been reported to associate with both strong or absent antral contractions.
Reliability of the EGG has been well
documented by comparing mucosal with serosal
electrodes.1 5–7 Reproducibility has been
demonstrated by the observation that the
amount of normal activity does not significantly
change if performed on separate days.8
Furthermore, the EGG is not significantly
affected by age or sex.
The pathogenesis of gastro-oesophageal reflux
disease (GORD) is multifactorial.10 Transient
relaxation of the lower oesophageal
sphincter and delayed oesophageal clearance
are important but gastric factors have also been
implicated.A number of studies have demonstrated
delayed gastric emptying for solids or
liquids in GORD but other studies have failed
to demonstrate this correlation.11 The inconsistencies
remain unexplained and the role of
gastric motility in GORD requires further
clarification. The EGG not only provides
information on gastric myoelectrical activity
but also predicts gastroparesis with an accuracy
of 78%.
Gastric dysrhythmias have been described in
a variety of disorders including functional dyspepsia,
motion sickness, nausea of pregnancy,
anorexia nervosa, and idiopathic and diabetic
gastroparesis.12–18 There is a report that the
EGG may be abnormal in elderly patients with
GORD.
The aim of this study was to investigate gastric
pacemaker activity in GORD. The study
was designed to assess the EGG both in
uncomplicated GORD and in a subgroup who,
in addition to GORD, had an additional
predominant symptom of food regurgitation.
To evaluate and compare GORD patients with
or without food regurgitation, the lower
oesophageal sphincter and oesophageal acid
exposure were also assessed.
Methods
Subjects prospectively studied included 40
patients with GORD and 30 asymptomatic
controls.GORD patients were characterised by
a clinical presentation of heartburn and/or acid
waterbrash. In all GORD patients the diagnosis
was confirmed by 24 hour oesophageal pH
analysis and/or the finding of oesophagitis on
oesophagogastroduodenoscopy. Within the GORD group there were 20 patients with typical
acid reflux symptoms and 20 patients with
the additional symptom of food regurgitation.
The regurgitation patients were characterised
by a predominant complaint of involuntary
solid or semisolid food regurgitation into the
mouth. All patients had an oesophagogastroduodenoscopy
performed. Patients with
Barrett’s oesophagus, oesophageal ulceration,
stricture, or malignancy were excluded from
the study. The control group consisted of
healthy individuals who did not complain of
gastrointestinal symptoms.
The EGG was performed following a six
hour fast. Any medication with potential to
influence gastric motility or acid production
was discontinued for at least 48 hours before
the motility recordings. Patients were studied
in a semireclining position and requested to
avoid major movements. The skin was lightly
abraded with gauze prior to placement of the
adhesive gel EGG electrodes. Two bipolar skin
electrodes were placed on the abdomen; one
midway between the xyphoid process and
umbilicus, and the other 5 cm to the left, just
below the costal margin. A reference electrode
was placed on the right side of the abdomen.20
The electrodes were connected to an EGG
recording unit (Synectics, Stockholm, Sweden).
A one hour fasting recording was
performed after which the patient drank 150
ml of water and ate a standardised cheese salad
sandwich (575 kcal; 50% carbohydrate, 25%
protein, 25% fat). This was immediately
followed by a one hour postprandial recording.
A standard method for data analysis was
performed. The EGG data were analysed by
the “multigram” Synectics software package
running on a personal computer. A sampling
frequency of 4 Hz was used. The EGG analysis
is based on the fast Fourier transform (FFT)
technique. A data period of four minutes and
16 seconds is analysed and termed an FFT
line. The dominant frequency for each FFT
line is calculated and consecutive data periods
are displayed by running spectrum analysis.
The FFT lines are displayed at one minute
intervals, which corresponds to an overlap of
three minutes and 16 seconds between data
sets for adjacent FFT lines. For the periods
before and following the test meal, an average
FFT line is calculated, from which the power of
the dominant frequency is derived. Prior to
analysis of the EGG signal, visual inspection of
the waveform detected any obvious major
movement artefacts. These were defined as
abnormally large positive and/or negative peaks
in the tracing and were deleted from the analysis.
Due to overlap of data displayed as FFT
lines, a major movement artefact results in
deletion of approximately five minutes of data.
Normal electrical activity was defined as a
frequency of 2–4 cycles per minute. Activity of
0–2 cycles per minute was termed bradygastria
and 4–9 cycles per minute as tachygastria. An
abnormal EGG was defined as <70% normal
electrical activity either before or after the test
meal. The power (or amplitude) of the
dominant frequency was measured both before
and following the test meal, and the postprandial
to preprandial power ratio was calculated.
The stability of the EGG frequency before and
after food was calculated, and expressed as a
dominant frequency instability coefficient.
The lower oesophageal sphincter was assessed
by standard oesophageal manometry
performed following a six hour fast. A four
channel water perfused system (Synectics,
Stockholm, Sweden) was used with the patient
positioned in the supine position. Mean end
expiratory pressure and mean total and abdominal
lengths of the lower oesophageal
sphincter were recorded by a stationary pull through technique. Oesophageal peristalsis was
studied using 10 swallows of 5 ml of water.
Severity of oesophageal acid exposure was
measured by 24 hour oesophageal pH analysis.
A pH sensor was placed 5 cm above the proximal
border of the lower oesophageal sphincter
following manometry. In addition to other
restricted medications, proton pump inhibitors
were discontinued at least five days prior to pH
recording. The sensor was connected to an
ambulatory recording unit (Synectics, Stockholm,
Sweden) and patients were instructed to
follow their normal daily routine. Dietary
restrictions in the test period included alcohol,
caffeine containing beverages, citrus drinks,
and chocolate. Oesophageal acid exposure was
assessed using the Demeester score.23 An
abnormal score was considered when the score
was >14.72.
EGG data were expressed as median (interquartile
range). Manometry and 24 hour pH
data were expressed as mean (SD). Nonparametric
data were analysed by the Mann-
Whitney U test. Parametric data were analysed
by the Student’s unpaired t test and Fisher’s
exact test. Statistical significance was taken as
p<0.05.
Results
Mean ages in the patient groups were: controls
27 years; acid reflux 42 years; and food regurgitation
52 years. Female/male ratios were:
controls 17/13; acid reflux 14/6; and food regurgitation 8/12. A Demeester score >14.72 was
recorded in all acid reflux patients and in 13/20
food regurgitation patients. There were seven
food regurgitation patients who did not undergo
pH monitoring, and all had oesophagitis on
oesophagogastroduodenoscopy. Oesophagogastroduodenoscopy
showed no other significant
mucosal disease except that two patients with
acid reflux and 13 with food regurgitation had
Savary-Miller grade 1–2 oesophagitis. No laryngeal
or pharyngeal inflammation was seen in any
patient.
An abnormal EGG was defined as <70%
normal electrical activity either before or after
the test meal.13 22 Eight asymptomatic controls
(27%) demonstrated a postprandial power
reduction and this was not considered to indicate
an abnormality in the absence of a significant
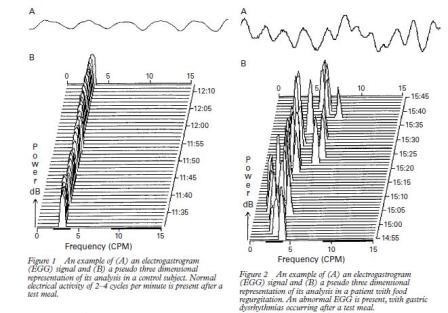
dysrhythmia. Figure 1 shows an example
of a pseudo three dimensional representation
of an analysed EGG in an asymptomatic
control subject. The electrical activity was
stable and did not change significantly after a
standard test meal.
An abnormal EGG was present in two (7%)
asymptomatic controls, two (10%) GORD
patients with acid reflux, and 10 (50%) GORD
patients with food regurgitation. GORD patients
with food regurgitation, but not solely acid
reflux, were significantly more likely to have an
abnormal EGG compared with asymptomatic
controls (p<0.001). Figure 2 shows an example
of a pseudo three dimensional representation of
an EGG in a patient with food regurgitation,
demonstrating abnormal pacemaker activity
throughout the recording.
EGG parameters were analysed individually
(table 1). GORD patients with only acid reflux
did not differ significantly in any EGG parameter
compared with controls. In contrast,
GORD patients with food regurgitation had
significantly more tachygastrias both before
(p<0.02) and after (p<0.01) the test meal.
Regurgitation patients also had a more unstable
electrical frequency (calculated as the
dominant frequency instability coefficient) following
the test meal (p<0.003).
Oesophageal manometry and 24 hour pH
data were available for analysis in all GORD
patients with acid reflux and in 13/20 with food
regurgitation (table 2). Oesophageal motility
disorders were found in four patients with acid
reflux (three non-specific, one sclerodermalike
oesophagus), and two regurgitation patients
(two non-specific). GORD patients with
food regurgitation and an abnormal EGG had
higher oesophageal acid exposure than those
with a normal EGG (p<0.05). When food
regurgitators with normal and abnormal EGG
were compared, no difference in any lower
oesophageal sphincter measurement was observed.
However, a 1:1 association between
severity of oesophageal acid exposure and an
abnormal EGG was not apparent, as some
patients with severe GORD had a normal
EGG.
Discussion
This study has documented the prevalence of
EGG abnormalities in GORD. Abnormality of the EGG depends on the nature of the refluxate
material. Half of the GORD patients complaining
of food regurgitation had an abnormal
EGG while in those with solely acid reflux
there was no difference in gastric pacemaker
activity compared with asymptomatic controls.
Regurgitation patients had significantly
more tachygastrias both before and after a test
meal. Tachygastrias have been shown to correlate
with antral hypomotility.1 2 The findings
suggest that half of patients with food regurgitation
have associated antral hypomotility.
Half of patients with food regurgitation had a
normal EGG. The reason for this is unclear
but may reflect either a different pathogenesis
or that in these patients gastric dysrhythmias
are transient and were not detected at the time
of testing.
GORD patients with food regurgitation and
an abnormal EGG had significantly greater
oesophageal acid exposure than those with a
normal EGG. There was no significant difference
in the lower oesophageal sphincter
between food regurgitators with normal and
abnormal EGG suggesting that gastric dysrhythmias
add to the degree of acid reflux.
However, a large amount of oesophageal acid
exposure was not always associated with an
abnormal EGG, supporting the concept of a
multifactorial pathogenesis for GORD.
The observation that gastric pacemaker
activity may be abnormal in food regurgitation
suggests that an antroduodenal motility disorder
might be a confounding factor in these
patients. Antroduodenal manometry is invasive
and an abnormal EGG may act as a screening
test to define patients where further testing is
justified. This requires further study.
This study excluded patients with Barrett’s
oesophagus and benign oesophageal strictures.
These subgroups deserve further study. Antropyloroduodenal
incoordination when combined
with gastro-oesophageal reflux may
cause regurgitation of bile into the oesophagus.
10 This is a suggested pathogenic mechanism
in Barrett’s oesophagus.24 The EGG may
therefore shed further light on the pathogenesis
of complicated GORD.
Identification of EGG abnormalities in
GORD patients may also have implications for
treatment. The prokinetic agents cisapride and
domperidone have been reported to improve
EGG abnormalities in functional dyspepsia
and gastroparesis.25–28 These types of agents
may have a particularly useful role in GORD
patients with food regurgitation.
|